Heart disease is frequently seen in both dogs and cats. There are many types and causes of heart disease and they can occur from birth to old age. Like many other illnesses, it is important to diagnose and treat heart disease as early as possible to ensure our pets live without symptoms of illness for as long as possible.
Inherited or Congenital Heart Disease
Heart disease in dogs and cats can be congenital/inherited or acquired. Congenital disease can cause malformations of the heart which impairs function and can be present at birth. Hereditary disease can cause congenital problems or increase the likelihood of adult-onset heart disease, particularly heart muscle diseases in both dogs and cats.
Your pet’s breed may have increased chances of having inherited diseases. Some cat breeds that are predisposed to heart disease include the Maine Coon Cat, Siamese, British Shorthairs, and Persians.
Examples of dog breeds with increased chances of heart muscle disease are Cocker Spaniels, Boxers, Doberman Pinschers, and other large to giant breed dogs.
Acquired Heart Disease
Other kinds of heart disease can occur later in life related to other illnesses such as hyperthyroidism (particularly in cats), long term untreated dental disease, bacterial infections, and cancer.
What is the structure of the heart and how is it affected by heart disease?
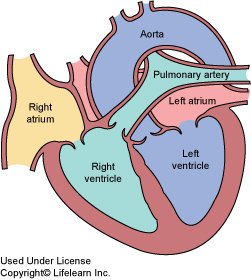
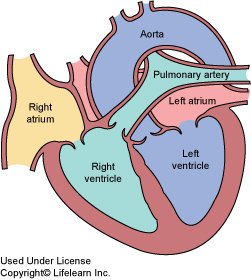
The heart can be divided into 4 functional components:
1. The heart muscle which pumps the blood around the body
2. The heart valves which act to prevent the blood going in the wrong direction
3. The pericardium which is a tough membrane surrounding and protecting the heart
4. The electrical conducting system which acts to initiate and transfer electrical impulses around the heart allowing it to contract or “beat” in a systematic and coordinated fashion
Any or all of these parts can be affected by heart disease.
What are the signs of heart disease in cats?
Most cats do not display any clinical signs until the disease is advanced. Unlike humans and dogs with heart disease, cats rarely cough if they have heart disease. Exercise intolerance does occur but can be difficult to recognize since cats rarely go for walks or engage in sustained physical activity with their owners. With advancing disease and declining exercise tolerance, cats tend to become more withdrawn, hide under furniture and sleep more.
The most common signs of heart disease in cats are:
- poor appetite
- weight loss
- lethargy
- increased respiratory rate and effort
- sudden collapse
- sudden hind leg paralysis accompanied by pain
- stunted growth (kittens)
Common signs of heart disease in dogs
The most common clinical sign of congestive heart failure (CHF) is persistent coughing accompanied by difficulty breathing. This is due mainly to pulmonary edema or the accumulation of fluid in the lungs. The enlarged heart will also push against the trachea, causing irritation that can induce a cough. Many dogs with CHF will fatigue more easily, have reduced stamina and not engage in playing or walking as they once did. Coughing when at rest or sleeping, excessive panting, persistent loss of appetite, a swollen belly, and pale or bluish gums are also signs associated with heart failure. The dog will develop generalized weight loss and muscle wasting due to the effects of CHF on other body systems. If any of these signs develop in a pet with a heart murmur, notify your veterinarian immediately.
How is heart disease diagnosed?
As mentioned above, early diagnosis is very important, since our patients hide signs of illness until the heart has advanced disease. Regular examinations are very important to detecting heart disease early. Puppy and kitten exams, yearly adult exams, and twice yearly senior (over 7 years old) exams are very helpful in diagnosing and treating patients before too much damage has occurred.
With any heart problem, diagnosis involves several tests:
Auscultation or listening to the heart with a stethoscope is the first step in diagnosing heart disease. Heart murmurs are detected by auscultation; the murmur’s location and intensity helps determine its significance. The heart rhythm is assessed, and if there are concerns, the veterinarian may simultaneously palpate or feel the pulse to determine its strength and rhythm. Finally, the lungs are assessed, looking for evidence of changes associated with heart failure.
Chest x-rays are taken to evaluate the size and shape of the heart and look for lung changes such as the presence of fluid as in CHF.

Blood and urine tests are performed to give an indication of any other disorders in the body. Liver and kidney function are often impaired in patients with heart disease.
An electrocardiogram (ECG) measures the electrical activity of the heart and allows accurate determination of both heart rate and rhythm. Any abnormal rhythms (arrhythmias or dysrhythmias) can be detected and evaluated.
Ultrasound examination (echocardiogram) utilizes ultrasound waves to evaluate the heart. The size and thickness of each heart chamber can be evaluated, and the effectiveness of the heart’s contractions can be directly observed. Measurements can be taken to evaluate the heart’s pumping efficiency.

Can’t you treat my dog without these tests?
Accurate diagnosis gives us a much better guide to the type and extent of treatment necessary. Today there is a wide selection of heart medications that can be used to treat congestive heart failure and treatment regimes must be tailored for each patient. Without these tests, your veterinarian is unable to determine the optimal treatment for your pet, and may inadvertently cause more harm than good. With proper treatment, many dogs are able to live a normal life for many months to years.
Ernest Ward, DVM © Copyright 2009 Lifelearn Inc. Modified by Dr. Clouse with permission under license.